 Technology
Technology  Ultraviolet light can kill almost all the viruses in a room. Why isn’t it everywhere?
Ultraviolet light can kill almost all the viruses in a room. Why isn’t it everywhere? January 17, 2024:
As I write this article, I have a cold.
At some point in the past couple of weeks, I managed to inhale a droplet of water suspended in the air that contained hundreds or thousands of copies of a virus (probably a rhinovirus, the kind that causes most common colds). That virus infected my throat and my sinuses, resulting in the sore throat and stuffed-up nose I have right now.
As inconveniences go, this feels rather minor. I think of my friends with small children, who are constantly careening between RSV and the flu and god knows what other infection their kids picked up in day care and brought back home. I think of my family in assisted living facilities, who sometimes find themselves confined to their rooms, unable to see their friends or interact with the outside world, when there’s a respiratory virus going around. I think of the roughly 1.3 million people a year who die of tuberculosis, a respiratory bacterium that we have yet to defeat. And, of course, I think of the 7 million or so people worldwide killed over the past four years by a respiratory virus spread this exact same way: Covid-19.
At least as long as human beings have lived in large, close groups, respiratory viruses have been present — sometimes an annoyance, sometimes a catastrophe. Though we’ve managed to create vaccines and drugs to blunt their effects, the viruses endure.
But there is a group of people who think we do not need to live this way. These scientists, activists, and entrepreneurs believe we’re going to look back on this era, one of commonly endured airborne infections, as a case of antiquarian barbarism, a bunch of needless suffering that we accepted because we didn’t know any better. They believe that we have the technology now, and will have even better technology soon, that could end respiratory infections for good, the way that disinfecting our drinking water with chlorine helped end typhoid as a major cause of death in the US.
The technology is called germicidal ultraviolet light (GUV), and in particular, a relatively novel kind of ultraviolet light often denoted as “far-UV.” “We have so much data suggesting that this is far and away the most impactful technology, when it comes to protecting people from infectious disease, that exists today,” says Kevin Esvelt, a professor and biologist at MIT who has championed the idea.
These advocates imagine a world in which far-UV lamps are set up in most large indoor spaces where people gather, emitting rays that kill airborne viruses and bacteria while leaving humans unharmed. If all goes according to plan, day cares will stop spreading around noroviruses and flus; hospital infections will plummet; elderly and immunocompromised people can gather openly, unmasked, without fearing they’ll catch something. In a world where the flu alone imposes an average of $11 billion in economic costs per year to the US and Covid has cost the United States on the order of $14 trillion, it’s a nearly utopian vision.
The next Covid would be strangled in the crib, unable to reach the billions of people SARS-CoV-2 did because it’s deactivated at every turn. Unlike a vaccine, which needs to be formulated anew for every emerging pathogen and then proactively taken by everyone at risk, far-UV would be a passive defense against respiratory viruses of all sorts, existing ones as well as those to come. Pandemics would go from a regular threat to a thing of the past.
That’s the plan, anyway. But there’s still a lot we do not know, not least about what shining these lights does to the air it touches and what that could do to humans who breathe that air. It’s a technology with incredible promise, but one where getting the details right could hardly be more crucial.
Humans can see waves of electromagnetic radiation with wavelengths between about 400 to 700 nanometers (a measurement that is one-millionth the size of a millimeter), with violet colors coming at the shorter end of that range and red at the longer end. This is what we know as “visible light.” Radiation with wavelengths just longer than this is called “infrared”; go longer still and you get radio waves. Radiation with wavelengths just shorter than visible light is called ultraviolet; go even shorter and you get X-rays. Ultraviolet light is subdivided into UV-A (315 to 400 nm), UV-B (280-315 nm), and UV-C (100-280 nm). Artificial UV used for disinfection is almost always UV-C, so UV and UVC are often used interchangeably as terms in public health.
Most people know of ultraviolet radiation as a health risk — which it can be. It causes sunburns and skin cancer if encountered in large quantities; sunscreen blocks it. But UV radiation isn’t all bad: In milder quantities, it also allows skin to produce vitamin D. And for nearly a century and a half, researchers have known that ultraviolet light can kill viruses and bacteria, for the same reason it can damage skin cells. Sunlight is, if not the best disinfectant, a quite good one.
In 1877, the researchers Arthur Downes and Thomas Blunt published a note in Nature stating that sunlight in small doses stopped bacteria from reproducing, and in larger amounts killed off the pathogens altogether. A follow-up paper by the two the same year concluded that the effect was “chiefly … associated with the actinic rays of the spectrum,” “actinic” being an archaic term for “ultraviolet.”
The husband-and-wife team of William F. Wells, an engineer and renowned oyster breeder, and physician Mildred Weeks Wells picked up the hunt in the 1930s. In 1935, William Wells and Gordon Fair published an article in Science documenting that an ultraviolet lamp placed in a room completely killed off bacteria in the air.
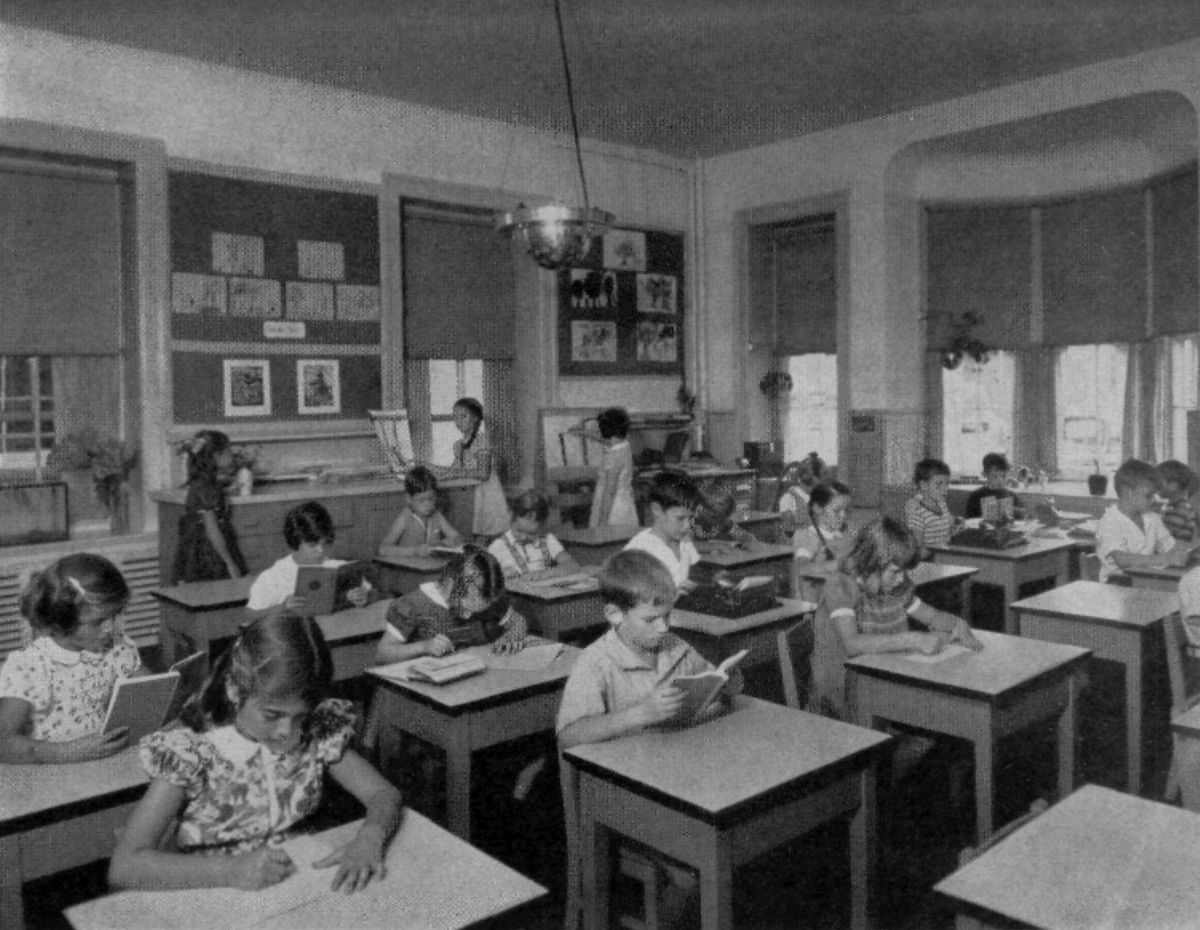
The Wellses and Penn professor T.S. Wilder conducted a pilot at Germantown Friends, a private school in Philadelphia, to see if UV radiation could prevent disease in a real-life setting. They placed “irradiation chambers” under the ceilings of classrooms; air would naturally travel up to the chambers, where it would be subjected to UV rays meant to kill off pathogens. The results were striking: In classrooms with the radiation, only 14.5 percent of students were infected with measles during a 1941 epidemic of the virus. (This was decades before the measles vaccine was invented.) In the non-irradiated classrooms of the school, 55.3 percent were infected. The Welleses conducted a second experiment in public schools in the suburb of Swarthmore, with similar results.
Subsequent research, however, was more equivocal. Nicholas G. Reed, author of a history of UV disease control, notes that the follow-up studies with weaker results can be explained by “infections occurring outside the classroom. … Wells successfully prevented the spread of measles in schools because infection occurring outside the school in a wealthy Philadelphia suburb was unlikely.” In the other trials, where participants were encountering airborne diseases in settings outside the one site with UV disinfection, just covering one of the places they went didn’t make a huge dent in illness.
At the same time, the increasing popularity of antibiotics and antiviral vaccines raised hopes that such measures by themselves would be sufficient to rid society of disease. Ultraviolet retained a small coterie of enthusiasts over the ensuing decades, focused narrowly on preventing transmission of tuberculosis — which has no reliably effective vaccine for adults — in its remaining hotbeds, like homeless shelters. The biggest test it received, the Tuberculosis Ultraviolet Shelter Study of 1997-2004, demonstrated that “upper room” UV, in which UV-emitting lamps are placed at least 6.9 feet above the floor where they can disinfect air without harming humans, was safe. But the trial was not able to determine if the method actually worked because not enough people in the shelters got TB. That was good for the residents but bad for the research.
The hyper-focus on TB was part of a broader trend in medicine against taking airborne transmission of viruses and bacteria seriously because of a conviction that only very small pathogens could be suspended in air, as “aerosols.” Bigger pathogens, the old dogma went, could only be spread as “droplets,” expelled during a sneeze or cough and traveling maybe 6 feet away from the infected person and no further, and not staying in the air. UV can disinfect surfaces where droplets land, too, but it’s a less effective tool for droplet-based infection.
This helped motivate the “6 feet away” rule from early in the Covid pandemic: The idea was that the virus could travel no further, so maintaining several feet of distance was sufficient to prevent spread. It wasn’t — detective work from scholars including Linsey Marr, Jose-Luis Jimenez, and Katherine Randall in the middle of the pandemic determined that this conclusion was based on a misinterpretation of the Wellses’ research that had somehow persisted for decades in the medical profession. Covid and other viruses thought to be “too big” to spread as aerosols over long distances really did spread through the air and not just as droplets.
The knowledge that Covid and other diseases could be literally surrounding us in the air, and that cleaning that air could be an effective way to fight them, set the stage for UV to make a comeback.
“Upper room” UV, the primary form of UV disease control tested to date, is a kind of compromise. The primary wavelength it uses, 254 nanometers, is dangerous to human skin and eyes if directly blasted at them. So, well, you don’t blast it directly at them. The next best thing is to put the lamps high up in a room, where they can kill pathogens at that height and spare the humans.
But this has its own disadvantages. Airborne pathogens, we’ve learned from researchers like Marr, Jimenez, and Randall, are all around us, not just on top of us. While air is constantly circulating, meaning that upper-room lamps should in theory be able to kill all the pathogens in a room eventually, it raises the question of whether they can kill them in time. Suppose you and I are standing in a room, and I cough in your direction — or even speak or sing in your immediate vicinity. The viruses I’m spewing could get to you before an upper-room lamp has time to kill them.
Installation is also a challenge, in part because it remains a niche technology, which means professionals without special training in UV cannot put it in your building for you without risking dangerous levels of exposure. “As it stands right now, when you order an upper-room lamp … somebody from this very small company has to come install it for you,” Gavriel Kleinwaks, who leads an initiative around UV at the public health and pandemic preparedness group 1Day Sooner, says. “It can irritate your eyes if it’s done incorrectly. … That really, really limits the current possible uptake rate for upper-room [UV].”

Far-UV, by contrast, uses shorter wavelengths — conventionally around 222 nm. It’s much easier to install: You just put up a few special lamps in a room, no specialists needed. And it’s much newer, only emerging as an option thanks to recent work by Columbia University medical physicist David Brenner.
“A potential donor approached the dean at Columbia a decade or so ago,” Brenner recalls. “Her husband had died of a surgical site infection.” Such post-surgical infections are easy enough to treat with antibiotics, but not if the bacteria is drug-resistant. The problem is that drug-resistant bacteria are becoming more and more prevalent, requiring an endless race to develop new antibiotics that attack bacteria in new ways so medicine can keep up.
UV offered a way around that problem. It kills viruses and bacteria indiscriminately, without relying on specific proteins or other structures in those pathogens. They don’t get a chance to evolve immunity. They might adapt, but only over an extremely long time scale.
The problem is that you can’t safely shine conventional 254 nm light at humans, much less at the wounds of humans who are recuperating from surgery. So Brenner and his colleagues, thinking about the donor’s challenge, arrived at the idea of trying out shorter wavelengths, 207 nm or 222 nm far-UV. Those wavelengths penetrate far less than conventional UV, and because of that, far-UV seemed much less likely to damage human skin or eye cells, while still being strong enough to kill viruses and bacteria.
The ensuing decade of studies produced strong evidence that far-UV is both effective at killing viruses and bacteria and safe for human exposure. One of the more promising trials to date examined a room in which researchers continuously released airborne Staphylococcus aureus bacteria — the germ that causes staph infections. They then saw whether five far-UV lamps, operating at low power, could effectively kill the pathogen. It could. Even with more bacteria constantly spewing in, the far-UV reduced its prevalence by 98.4 percent. Unlike upper-room UV, the lamps could be pointed safely downward, killing viruses and bacteria in real time as people cough and talk.
It’s not just staph. Brenner and colleagues Manuela Buonanno, David Welch, and Igor Shuryak showed in 2020 that even low doses of far-UV radiation could kill 99.9 percent of coronaviruses in a test chamber. Two years earlier, they and other co-authors found it was over 95 percent effective against H1N1, or swine flu. With any disease they put against it that spread through the air, it just worked.
There are two major safety risks to humans from UV exposure: damage to skin and damage to eyes. But our skin and eyes are pretty resilient, and far-UV researchers were hopeful that our natural defenses would prevent any damage from short-wavelength radiation, which doesn’t penetrate the skin as deeply as long-wavelength radiation. “On the very surface of our skin, we have a layer called the stratum corneum, which is a layer of dead cells,” Brenner explains. “That’s, on the scale of things, pretty thick. We figured the far-UVC couldn’t penetrate that. Likewise, in the eye, the outer part of the eye is the cornea. But external to the cornea is the tear layer, which is a layer of liquid.” Far-UV, the hypothesis went, couldn’t penetrate that either.
So far, safety testing has borne out these predictions. Exposing the skin of hairless mice to 222 nm UV didn’t cause any skin damage. The physicist Ewan Eadie, then a researcher at the University of Dundee, exposed his own skin to the spectrum and found no reddening of any kind suggesting serious damage. At about 6,000 millijoules per centimeter squared, he started to see superficial yellowing without damage to any lower layers. That, for reference, is hundreds of times more radiation than produced by the lamps that killed off 98.4 percent of staph bacteria in a large room. In the real world, this just doesn’t look like a problem.
The evidence on eyes is more preliminary but also promising. A research team at Kobe University in Japan found that even after weeks of exposure, and even in mice that had been genetically engineered to be super-good at getting cancer, far-UV exposure led to “no significant changes on retinal tissue,” suggesting that, just as Brenner predicted, the watery outer layers of the eye absorbed the radiation without damage. (There was no significant skin damage, either — and no tumors, despite these being special cancer mice.)
Eadie and co-authors have looked at the eye question with humans. “We deployed the far-UVC into a classroom environment,” he told me. “We had three scenarios. We had a situation where the lamps weren’t on, which was our control. We had a situation where the lamps were on at 10 percent efficiency. And then we had the lamps that were on all the time at 100 percent efficiency.” Then, over a few weeks, they polled students, randomized in each of these arms, about their levels of eye discomfort. “What we found was that there was no difference at all in the reported discomfort between the control arm and any of the intervention arms.”
At this point, it’s clear that in small-scale settings, far-UV can kill the vast majority of pathogens present, which in turn would vastly reduce the risk of respiratory disease spread. It seems safe for human skin, and likely safe for human eyes, too. That’s what we know. What don’t we know?
“This is the most difficult talk I’ve had to give in my career,” Jose-Luis Jimenez, a distinguished professor of chemistry at the University of Colorado, told the audience at the first International Congress on Far-UVC Science and Technology this past June. “I’m not happy with the results, but they are what they are.”
Jimenez, who had done much to establish the importance of aerosol transmission during the apex of the Covid pandemic and thus understood the stakes of fighting airborne diseases as much as anyone, was there to tell the crowd they had a huge problem. Far-UV may be largely safe on human bodies, but it also created air pollution — substantial air pollution. And this pollution would be sufficiently bad for human health to seriously limit how many lives far-UV would save.
It’s a matter of fundamental chemistry. When far-UV light hits oxygen molecules, it breaks some of them to form O3 — better known as ozone. Ozone itself is hazardous, and responsible for about 365,000 deaths a year worldwide. Ozone also interacts with volatile organic compounds (VOCs), small carbon-based molecules suspended in the air. “When we paint or cook or put on shampoo, anything that smells is a volatile organic compound,” Jimenez explained to me. These compounds interact with the ozone to create particulate matter. And particulates in the air — smog, basically — can also kill. They kill some 6.6 million people annually, accounting for more than 11 percent of all deaths.
Everyone in the UV world knows this is a thing that happens when you put UV in a room. The question is one of magnitude: How big a problem is it? Jimenez argues that it’s significant. He estimates that if far-UV is installed in 1 percent of indoor spaces in the US, and without any increase in indoor ventilation, it could lead to “tens to hundreds” of extra deaths each year from air pollution.
In recent years, that toll pales in comparison to the toll from respiratory diseases. In 2020, the last year for which we have full data, about 404,375 Americans died of Covid or the flu. Reducing that by 1 percent would mean about 4,000 lives saved. Next to that, “tens to hundreds” of air pollution deaths might not seem like much. I certainly look at those numbers and think it’s a reasonable trade.
But 2020 was also an unusually brutal year for airborne disease: 49,783 Americans died from influenza in 2019, for instance (and none from Covid); 1 percent of that number is about 500 people, which starts to feel comparable to the air pollution cost Jimenez identifies. (In developing countries like Nigeria, where 125,000 people died of airborne TB alone in 2021, the benefits of disinfection may be higher.)
If you clean the air through better ventilation and filtration, the dangers of far-UV light are much smaller, but the benefits are also smaller, as the filtration is ridding the air of pathogens on its own, and the costs are higher. Jimenez favors using UV in very high-risk locations, such as hospitals, but worries that construction companies, schools, malls, and the like will seize on the potential of far-UV as an excuse not to invest in proper ventilation and filtration, leaving us with the ugly trade-off he identifies.
Still, many far-UV enthusiasts are highly skeptical that the trade-off is as significant as Jimenez believes. Brenner argues that Jimenez’s calculations are based on laboratory settings and don’t give a realistic sense of how much ozone would actually be floating around in a real-world situation. Ozone “gets absorbed in the walls, gets absorbed in carpets and so on,” Brenner says. “There have been a couple of studies now of far-UVC in a real-life room, one in an office and one in a hotel. And the levels there are way, way lower than you would see in a sealed metal chamber.”
Jimenez counters that the products of the ozone that is destroyed in those ways can be just as dangerous as ozone itself. But both researchers agree that we simply need to know more. We need more research to know just how serious a problem the air pollution generated by UV light is.
The next step for far-UV is also the next step necessary to settle the great ozone debate: a big, real-world pilot. Specifically, we need an oil rig.
“People typically work on them for a month, and then they go back to the mainland for a month,” says Esvelt, a hyper-cerebral biologist who’s maybe the last person I ever expected to explain to me how oil rigs work. “After two weeks, you usually have a shift. Half the crew leaves and their replacements come on. … That introduces a bunch of new pathogens, which then can circulate.”
If researchers were able to install far-UV lamps on the rig, they could measure the amount of pathogens circulating and test residents for various viruses over time. They could also monitor indoor air quality and see how much of the kind of particulate pollution that worries Jimenez shows up. Scientists could then compare to control oil rigs and see how much less disease, and maybe how much more ozone, shows up.
The hope among far-UV’s proponents is that a successful pilot like this, while potentially costing a few million dollars, could prove to businesses that it’s in their interest to buy lamps for their conference rooms, their hospitals, their classrooms. If it works, far-UV should reduce illness enough to make a real dent in absentee rates. Workers cost a lot of money; getting them to work more should be in the narrow, profit-seeking interest of most businesses.
“The cost of utilities [electricity, water, etc.] is about $3 per square foot for a facility,” P.J. Piper, founder and CEO of the lamp company Far UV Technologies, claims. “The cost of the facility itself is like $30 per square foot, but the cost of the people in the facility is more like $300 per square foot. … So even a 1 percent reduction in absenteeism is actually worth your entire utility budget, right?” And if far-UV meets its promises, the reduction could be much more than 1 percent. Piper is already selling lamps to varied clients, like a school district in South Carolina and the University of Maryland. A good pilot would expand his customer base dramatically.
A report from 1Day Sooner and the research group Rethink Priorities estimates that outfitting a room roughly 750 square feet in area with far-UV lamps currently costs between $2,500 and $5,000, depending on the shape of the space. That doesn’t include the cost of additional filtration to account for any ozone effects. But it’s much more cost-effective, in terms of disinfection per dollar, than using ventilation and filtration systems alone, an idea that has gained currency since the Covid pandemic began. And while increased ventilation brings significant energy costs, the energy usage of UV lamps is minimal.
All told, the report estimates that a comprehensive plan to improve air quality, including far-UV, upper-room UV, and ventilation/filtration, in every single commercial building in the US would require a one-off investment of $214 billion. That’s not a small amount, but if businesses can be convinced it’s in their interest to pay for a big share of it, that’d go a long way.
The hopeful scenario goes a bit like this: A big pilot shows that far-UV works; demand soars among rank-and-file businesses; and this makes it financially viable for businesses to invest in technological breakthroughs that could make far-UV lamps even better. A number of startups are working on so-called “solid-state UV,” produced through LEDs or other non-gaseous light sources. These sources are still experimental and not ready for large-scale commercial production. But if they work, they could experience price declines akin to those that ordinary LCDs and LEDs have experienced over the years, as TVs and computer monitors have ballooned in size and plummeted in cost.
That only happened because there were millions, perhaps billions, of customers lining up, willing to pay for those products. That isn’t yet true for far-UV. And making it true could be a crucial step in starting to make the far-UV dream of clean, germ-free air everywhere a reality.